Understanding the Industry: The Origins of Healthcare Administration
To know healthcare administration is to love healthcare administration
The most common misconception that I’ve encountered when talking about healthcare administration with others is that they think I mean “hospital administration”, when honestly, that could be the furthest from the truth.
But, this assumption is not completely misplaced.
Once upon a time, healthcare administration did mean hospital administration. In fact, there was a time where the former wasn’t as prominent and the two were essentially synonymous.
The Origins of Healthcare Administration
Before there was healthcare administration, which encompasses many more possibilities and career paths, there was hospital administration.
The modern concept of hospital administration traces back to the fall of 1899, when the Association of Hospital Superintendents was formed in Cleveland to bring hospital administrators together to establish medical practice guidelines. In 1906, the organization adopted a new name, The American Hospital Association (AHA), and made it easier for other hospital executives to join albeit without voting privileges1.
As the number of hospitals grew, it became more and more apparent that there had to be some type of training program to prepare individuals for management roles and would assume administrative responsibilities. Thus, the first modern day “Health Systems management program” was born in 1934 at the University of Chicago2. This eventually led to the first Master’s in Healthcare Administration degree program in the nation.
So, this entire career field originated from the healthcare industry moving towards creating curriculum and experiences to appropriately prepare students for administrating hospital departments and programs. Over the years, as the healthcare system began to grow beyond hospitals, so did the leadership and management positions.
Today, Healthcare Administrators work behind the scenes, managing your patient records, the inner politics of the hospital, the hospital’s finances, various administrative work, and more. In simple terms, I would describe this role as the Big Brothers & Big Sisters of the healthcare industry, watching over the welfare of entire hospitals, healthcare facilities, and other types of healthcare organizations.
This Wikipedia article claims that all of healthcare administration comes down to 2 categories: Generalist or Specialist…but, in my opinion, that too is furthest from the truth.
It started as Hospital Administration, but now it’s Healthcare Administration
When you consider the origins of this industry, you begin to understand why one might learn a simplified version of the American healthcare system.
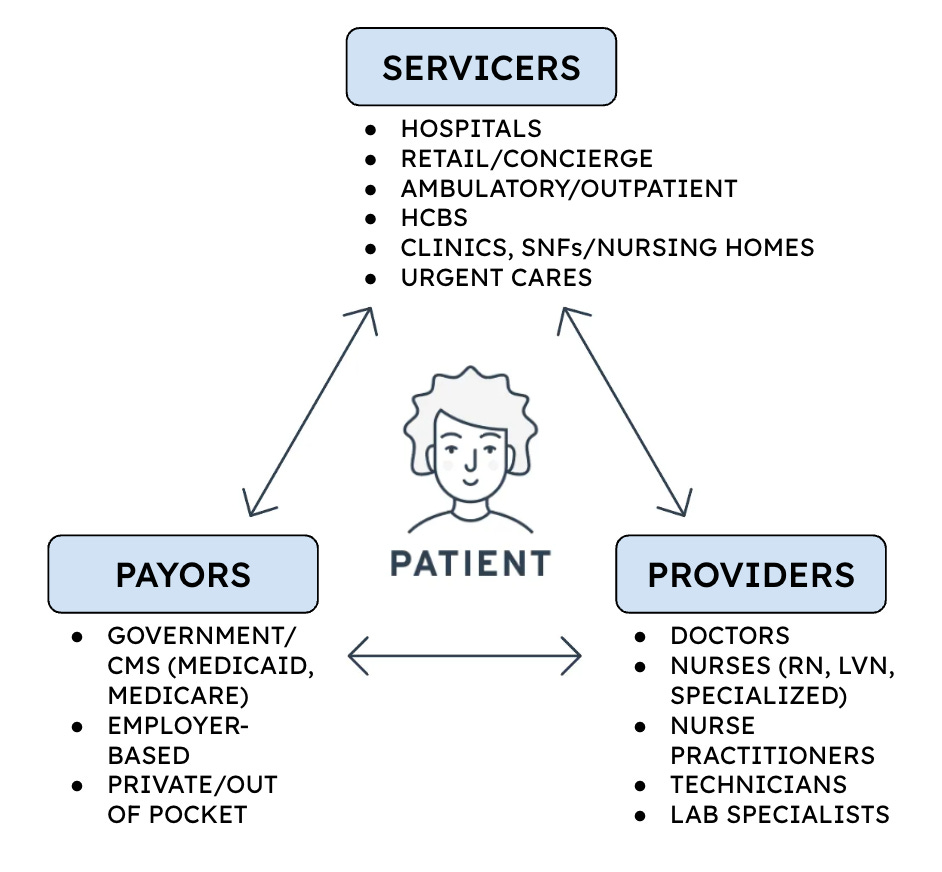
For example, take this diagram3 below:
This is the healthcare system that I was initially taught at the beginning of my college career. And at the time, a diagram like this really opened my eyes because previously I thought the only way to have impact on the healthcare industry was to be a Doctor or a Nurse.
Surprisingly, this diagram doesn’t mention hospitals - I would wager that this is because it’s presumed that patients receive medical treatment in a hospital. Several years ago, it wasn’t common for people to receive care in other settings (i.e. home-based care, ambulatory care).
For the majority of the modern American healthcare system’s lifetime, hospitals were considered critical to the entire model. It was a centralized place where people could receive care according to their health condition (from the not-so-bad to the very-bad) and be monitored 24/7 by licensed healthcare professionals.
Back in the day, someone might ask: “Why wouldn’t you want to go to a hospital?”
Of course, if you belonged to any marginalized group then it wasn’t as commonplace to immediately turn to hospitals for medical care. From the birth control pill trials in Puerto Rico to the non-consensual hysterectomies occurring in the deep South to the Tuskegee Syphilis Study to the mismanagement and mistreatment of those suffering during the AIDS crisis, many people had good reason to stay away from hospitals.
The push for value-based care and health equity opened up more entry points for patients to access care.
Perhaps other healthcare providers and professionals noticed a different turning point, but for me, it was the summer of 2020.
Not only was the nation struggling with an all-out pandemic, but also, the death of George Floyd and Breonna Taylor (and too many others) promulgated the persistent presence of racism, bias, and racial/ethnic discrimination. In that summer, I had never seen so many articles and think pieces centered on health disparities.
Since then, there has been a shift in language from “health disparities” to “health equity”. The image above4 from the Johns Hopkins Center for Health Equity does a great job of detailing the differences between the two terms.
Just before the Health Equity movement was revitalized, there was a lot of conversation around value-based care, which is the notion that healthcare organizations and clinicians should be held accountable for the quality of care they provide. Both of these movements worked together to expand the settings in which they could receive medical care.
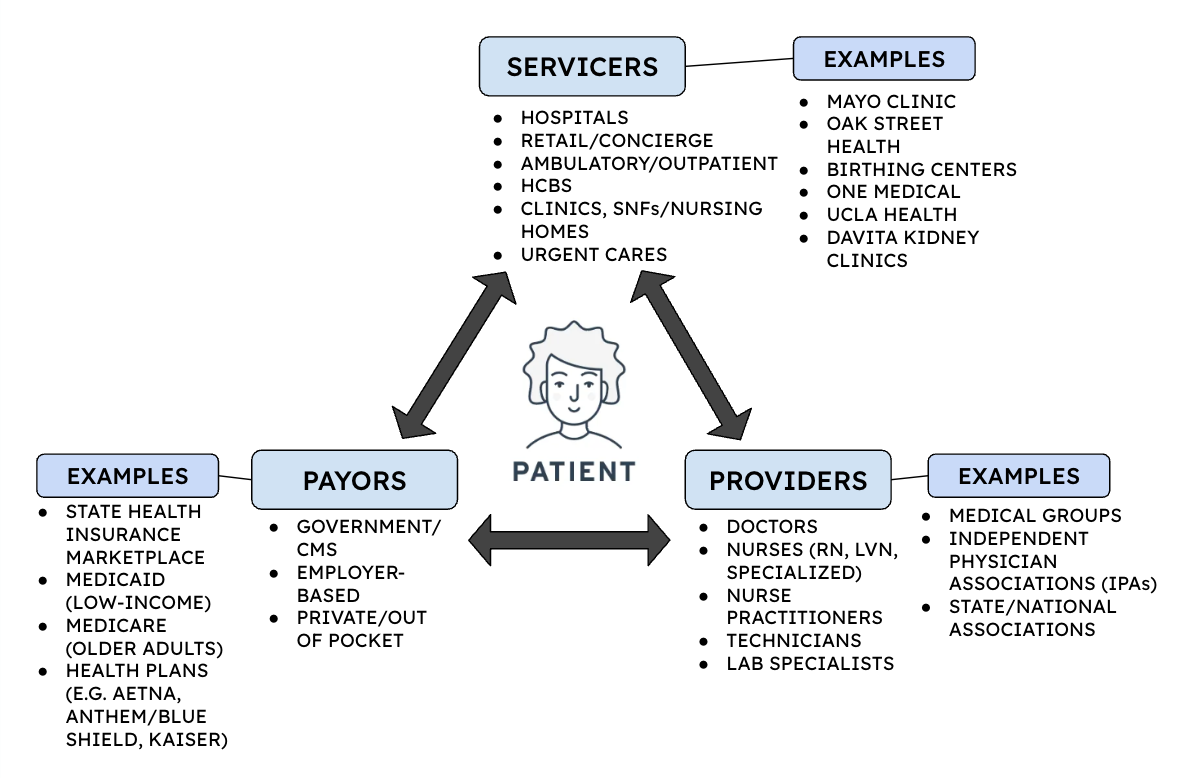
Today, the “Patient” sector of the healthcare industry is no longer synonymous with hospitals and has expanded to include Ambulatory Care offices, Retail & Concierge medicine, and Home and Community-Based services (HCBS) among many others.
Over the years, the “Payer” sector of the healthcare industry has also expanded with the onset of Medicaid, Medicare and the Affordable Care Act (ACA). Both expanded access to and the affordability of health insurance for many people across the country.
While the creation of Medicaid and Medicare allowed more individuals, specifically those that are low-income and elderly adults, to have health insurance, the Affordable Care Act lowered the burden of cost for those that still struggled to afford health insurance.
In California, the ACA (also known as Obamacare) enabled the creation of Covered California, which is a health insurance marketplace that holds health plans accountable, provides financial assistance to Californians, and assists with their enrollment into a health insurance plan.
And along with everything else, the type of providers as well as the places from which they provide services (or “Servicers” in the diagram) have expanded. Please see a more expanded view into the kinds of providers that operate within this sector below.
Now, the diagram is how I would describe the current state of the healthcare industry at a surface level perspective.
Servicers, Payors, and Providers are a great place to start when this is your first time trying to understand the healthcare industry. BUT - let me be clear that these are not the only sectors or areas that healthcare administrators can work in. In truth, this is just the first sphere which operates closest to the patient.
In the image above, I’ve expanded on this first sphere so you can get an idea of what each sector is as well as the corresponding organizations that you could work for with a Healthcare Administration degree.
Come back for the next edition to hear more about the secondary and tertiary spheres within the healthcare industry.
Don’t forget to share this post if you found it helpful!
AND - feel free to leave a comment down below if you want to start a conversation!
Source: The Key to Better Healthcare: Patient Power by Geoffrey Chaiken (July 2019) https://medium.com/@geoffreychaiken/the-key-to-better-healthcare-patient-power-5b371d4c2aa0
Source: Future of Nursing 2030 (August 2020) https://x.com/theNAMedicine/status/1296511712422699008